

Cirrhosis is the scarring of the liver – hard scar tissue replaces soft healthy tissue. It is caused by swelling and inflammation.
As cirrhosis becomes worse, the liver will have less healthy tissue. If cirrhosis is not treated, the liver will fail and will not be able to work well or at all.
Cirrhosis is caused by chronic (long-term) liver diseases that damage liver tissue. It can take many years for liver damage to lead to cirrhosis.
Chronic alcoholism is one of the leading causes of cirrhosis in the United States. Drinking too much alcohol can cause the liver to swell, which over time can lead to cirrhosis. The amount of alcohol that causes cirrhosis is different for each person.
Chronic hepatitis C is the another leading cause of cirrhosis in the United States. Hepatitis C causes the liver to swell, which over time can lead to cirrhosis. About one in four people with chronic hepatitis C develop cirrhosis. Chronic hepatitis B and hepatitis D also can cause cirrhosis.
Fat build up in the liver that is not caused by alcohol use, is called Non-Alcoholic Fatty Liver Disease (NAFLD), which can lead to nonalcoholic steatohepatitis (NASH), now called metabolic dysfunction associated steatohepatitis or MASH. NASH can cause the liver to swell and can lead to cirrhosis. People with NASH often have other health issues including diabetes, obesity, high cholesterol, coronary artery disease and poor eating habits.
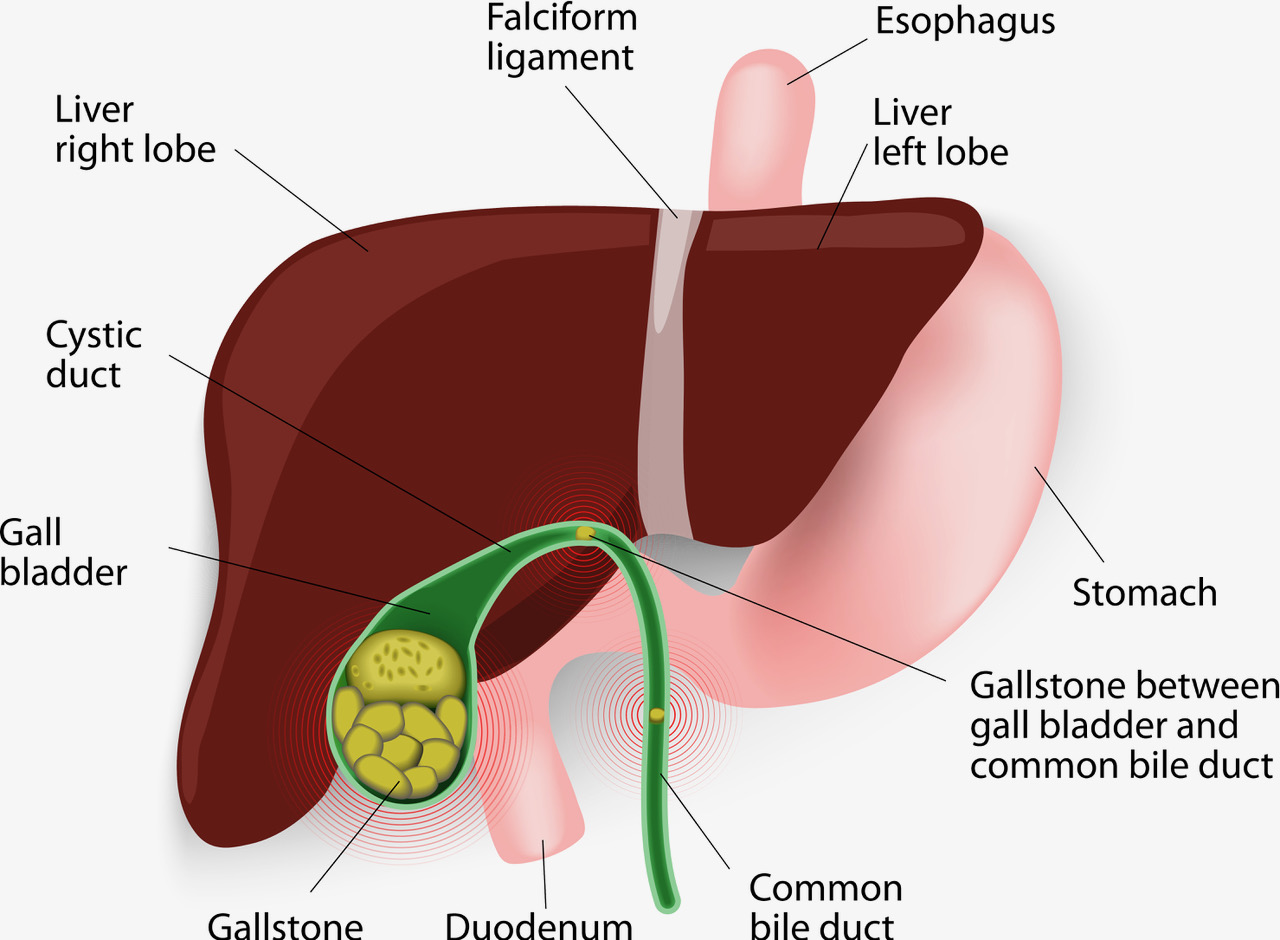
Bile duct disease limits or stops bile from flowing to the small intestine. The bile backs up in the liver causing the liver to swell and can lead to cirrhosis. Two common bile duct diseases are primary sclerosing cholangitis and primary biliary cirrhosis.
Some genetic diseases can lead to cirrhosis. These diseases include Wilson disease, hemochromatosis, glycogen storage diseases, Alpha-1 antitrypsin deficiency, and autoimmune hepatitis.
There are usually no symptoms of cirrhosis in its early stage. Over time, cirrhosis may cause symptoms and complications:
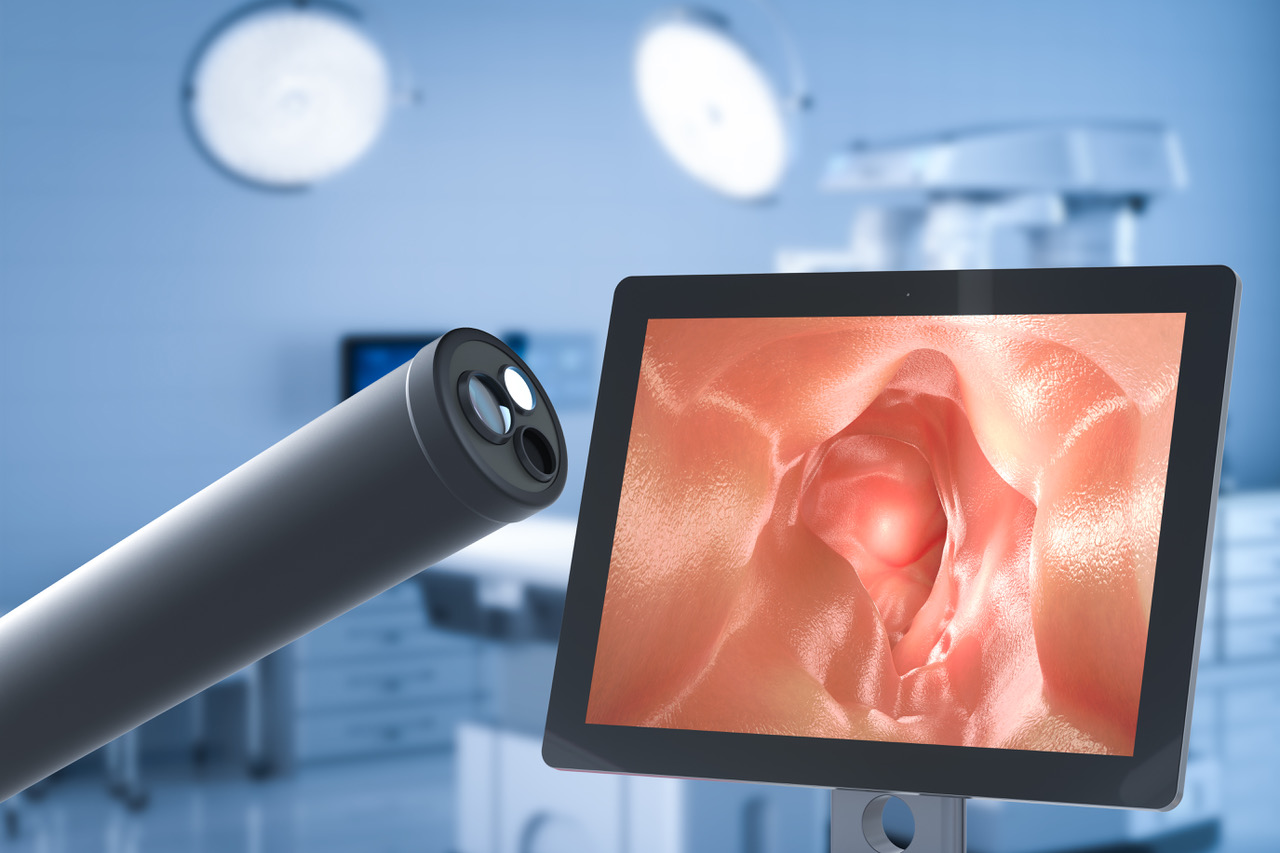
Cirrhosis is diagnosed by symptoms, blood tests, medical history, and physical examination. A liver biopsy may be needed to check how much of the liver has been damaged. During a biopsy, a small piece of liver tissue is removed and studied in the lab, and additional imaging may be needed.
Treatment options for cirrhosis depend on the cause and the level of liver damage. Depending on the disease causing cirrhosis, medications or lifestyle changes may be used for treatment. The goals of treatment are to prevent further liver damage and reduce complications.
When cirrhosis cannot be treated, the condition is known as End-Stage Liver Disease, or ESLD. ESLD includes a subgroup of patients with cirrhosis who have signs of decompensation that is generally irreversible with medical management other than transplant. Decompensation includes hepatic encephalopathy, variceal bleed, kidney impairment, ascites, lung issues. The decompensated liver disease allows these ESLD patients to be prioritized on the transplant list.
It is possible to prevent further liver damage with proper management of cirrhosis.











Contact Us
Covina Location
500 W. San Bernardino Rd, Suite B Covina, CA 91722
(626) 960-2326
Glendora Location
415 W. Route 66, Suite 102 Glendora, CA 91740
(626) 610-2112